Sunday, August 12, 2012
Friday, July 27, 2012
Acute testicular/scrotal pain
History & Physical Exam
- Pain? Acute onset suggests torsion, epididymitis, or torsion of the appendix testis/epididymis
- Trauma?
- Change in size? Valsalva = hydrocele
- Sexually active? Epididymitis in adolescents
- Difficulty voiding? Think mass, cord lesion, UTI
- Flank pain or hematuria? Referred pain from a kidney stone
- Abdominal pain, nausea/vomiting? Torsion
- Setting the stage
- Get a chaperone if you or patient are uncomfortable
- Have the patient stand if possible
- If you suspect a varicocele examine the patient supine as well
- Respect the patient’s privacy!
- Don’t forget to examine the;
- Inguinal folds
- Penis and urethra
- Pubic hair
- Testicular position (left is lower)
- Testicular lie
Testicular torsion
- Surgical emergency!
- The testicle twists on the spermatic cord
- Venous compression then…
- Edema of testicle and cord then…
- Arterial occlusion then…
- 1/4000 males < age 25
- Bimodal - neonatal and puberty
- 65% between ages 12-18 years
- Likely due to increasing testicle volume
- Bell clapper deformityTestis is not fixed to the tunica vaginalis posteriorly and it is free to rotate and is at increased risk of torsion.Incidence is approximately 1/125 and usually present bilaterally.
- Presentation
- Abrupt onset of pain <12 hours
- Associated N/V, lower abdominal pain
- In a retrospective review only 8% had pain prior to this episode (Kadish, 1998)
- Exam
- Edema of scrotum
- Testis – tender and slightly elevated, may have a horizontal lie
- Cremaster reflex is absent
- Torsion is ideally a clinical diagnosis
- If suspected tell your Attending and call Urology ASAP
- Ultrasound
- Sensitivity 69-100%
- Specificity 77-100%
- Nuclear medicine scans are very sensitive and specific – but not readily available
- Surgery
- If viable – detorsion of affected testis and fixation (orchiopexy) of both testis
Viability rates
Within 4-6 hours 100%
12-24 hours 20%
>24 hours 0%
- Sequelae
- Males may have increased risk of infertility even when viable de-torsed testis is left in scrotum because of immune-mediated injury to contralateral testis
- Other studies have failed to show that anti-sperm antibodies are present
- Intermittent torsion
- 80% have bell clapper deformity
- Pain is brief and resolves quickly (minutes)
- Eaton et al, 26% had nausea and vomiting, 21% pain awakened patient from sleep
- Neonatal torsion
- A topic that could have its own talk
- Many cases occur in utero
Torsion of the appendix testis and appendix epididymis
- Vestigial structures
- Appendix testis: Müllerian system
- Appendix epididymis: Wolfian system
- They torse easily
- Boys 7-12 years of age
- Pain is usually less severe
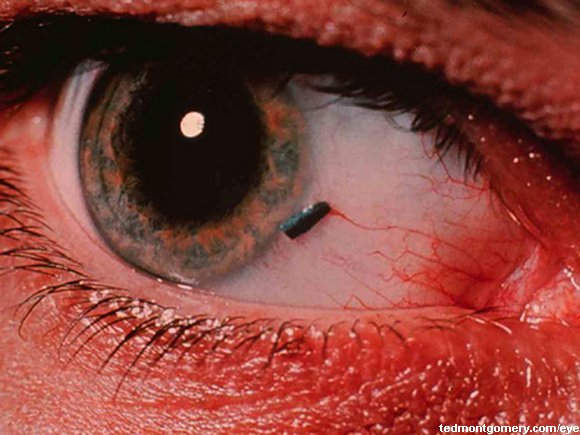
- The ‘blue dot sign’ is the pathognomonic physical finding
- Due to infarction/necrosis of the appendix
- A reactive hydrocele may also be seen
- Diagnosis
- Usually clinical if you see a ‘blue dot sign’
- Get an Ultrasound in cases where you can’t r/o torsion
- Management
- Analgesics
- Rest
- Scrotal support
- The pain typically resolves in 5-10 days
Epididymitis
- Etiology
- Sexually active? Chlamydia, gonorrhea, E.coli, viruses
- Prepubertal? Viruses, E. coli, mycoplasma
- Presentation
- Pain and swelling localized to the epididymis
- Testis has a normal lie
- 50% have scrotal edema
- The scrotum is sometimes red
- Cremaster reflex is present
- Positive ‘Prehn sign’ (not reliable)
- Patient may have dysuria
- The work-up
- Clinical exam
- Ultrasound
- Urinalysis
- Obtain in ALL patients with suspected epididymitis
- STD testing
- Get gc/chlamydia DNA of urine if sexually active
- Syphilis and HIV testing
- Prepubertal boys
- Antibiotics are NOT always indicated
- Treat if.. Pyuria >3-5 wbc, positive U/C, or underlying UTI risk factors - TMP/SMX or Cephalexin for 10 days
- Teenagers (Pro-Tip: think about STDs)
- Ceftriaxone 250mg IM x1 then doxycyline 100mg bid x10 days
- For enterics AND negative STD…
- 10 days of ofloxacin 300mg bid or levofloxacin 500mg qday
- Tx also includes rest, NSAIDs, and scrotal elevation
Tuesday, July 17, 2012
Academic Life in Emergency Medicine: Trick of the Trade: Converting % to mg/mL
Great quick tip here!
Academic Life in Emergency Medicine: Trick of the Trade: Converting % to mg/mL:
It's as simple as adding a zero - Seriously!
Academic Life in Emergency Medicine: Trick of the Trade: Converting % to mg/mL:
It's as simple as adding a zero - Seriously!
Friday, July 6, 2012
Ouch my eye! Ocular injuries in the pediatric ED
Here are some highlights from Eileen Murtagh-Kurowski's talk on ocular injuries on 7/6/12
Before moving on check out the PEMSHORT/CUTS video on using the Panoptic Ophthalmoscope
www.vimeo.com/pemcincinnati/panoptic
2. Always ask patients with eye infections whether or not they wear contacts
3. Use the panoptic ophthalmoscope for a much better view of the retina and fundus
Before moving on check out the PEMSHORT/CUTS video on using the Panoptic Ophthalmoscope
www.vimeo.com/pemcincinnati/panoptic
Corneal abrasions
Can only be diagnosed reliably with fluorescin under a Wood's lamp (black light). It may be advantageous to use tetracaine during the instillation of fluorescin. Otherwise saline will suffice. Fluorescin is safe to instill in any eye - even in an open globe. Please let your patients know that the tetracaine will burn during instillation. The treatment generally consists of topical antibiotics - I'll ask the parent which type (erythromycin ointment or polytrim drops) they would prefer. Generally corneal abrasions will heal well in less than a week, antibiotics can help reduce the already low risk of infection.Foreign bodies
Everting the top eyelid can allow you to visualize a foreign body which is usually behind the upper lid. Removal of material adherent to the inside of the upper lid can be done with a cotton swab, flush with saline, or needle nose forceps. Removing a foreign body off of the surface of the eye can be done (delicately) with an 18 Guage needle to 'flick' it off of the eye. Topical antibiotics are always appropriate.Abnormally shaped pupil
A pupil that is not a circle is bad. This generally indicates that the ciliary muscles of the iris have been disrupted/compromised. This can be due to direct trauma or an open blow.Traumatic iritis
Look for the patient with decreased visual acuity and extreme light sensitivity.Hyphema
Blood in the anterior chamber will create a meniscus like effect. These occur usually due to ocular trauma. The biggest risk is of acute angle closure glaucoma. The treatment is bed rest - for patients with a a hyphema >25-50% of the anterior chamber admission might be warranted. Rebleeding can occur - and the risk extends into and in some cases beyond the second or third day.The open globe
Generally fluorescin adheres to epithelium. Fluorescin that 'flows' is generally floating on the aqueous material. This is AKA Seidel's sign. The classic 'tear drop' shaped pupil is an important finding to recognize.Uveitis and hypopyon
White fluid in the anterior chamber - similar to a hyphema - is a hypopyon which can be infectious or inflammatory.General pearls
1. The visual acuity is the vital sign of the eye2. Always ask patients with eye infections whether or not they wear contacts
3. Use the panoptic ophthalmoscope for a much better view of the retina and fundus
Wednesday, June 6, 2012
To scan or not to scan - my thoughts
If you recall from my previous post we were considering when to get a head CT on a pediatric patient with a closed head injury, and specifically how to approach this with the family. In general I find that its best to be honest and discuss the criteria outlined in the Kuppermann article. Even if there is a parental expectation of a getting a head CT even before you enter the room, I've found that most parents understand where your coming form when you approach things in a straightforward and honest manner. They just want what's best for their kid - scan or not after all.
But what about those parents that still demand a scan for their child who is making shadow puppets with the otoscope light? First, it's important to address their concerns honestly and without pretension. Find out what they are worried about. Perhaps they had a family member who died in a car crash. Or just had an experience where "the doctors missed something." It's also important to remember that we aren't perfect diagnostic machines. Parents do know their children best. And on the flip side, if a situation seems fishy, especially in cases of suspected non accidental trauma, go ahead and get the scan.
The bottom line is that you should be familiar with how to explain the current evidence to your patients, and to openly acknowledge the risks, benefits, and parental concerns. Even with zero of the predictors for clinically important traumatic brain injury, there is still a 0.5% chance that the kid has a head bleed - even if they look perfect. Every parent - including this one - views their kid as one in a million.
Monday, June 4, 2012
To scan or not to scan - that is not the (only) question
Inspired by the cadre of closed head injuries that I saw in a recent shift I figured I'd launch phase 2.0 of The PEMTweets website with a discussion about how we manage closed head injuries in children. The issue I'll be addressing here is not one of when to scan or not to scan - that is an important decision that is now well supported by existing literature. Instead, allow me to focus on how we communicate our decision to an anxious family.
So, if you haven't already done so , go ahead and read the seminal Lancet 2009 article.
Kuppermann - Lancet, 2009
OK, welcome back... I ended up seeing three patients, all of whom presented by smacking their heads on hard surfaces. I've changed their names and ages to protect the innocent, and to avoid the wrath of Hungry Hungry HIPAA.
There is a delicate balance between managing the anxieties and expectations of a parent, when they are (justly so) legitimately worried about their child's well-being. Perhaps they are a medical professional themselves, and armed with just enough (mis)information to make them worry more than they should. Or maybe, they consulted Dr. Google, or worse, Dr. facebook in that back alley clinic that would make Dr. Nick Riviera of the Simpson's blush.
Go ahead and think for a moment about whether or not you would order a head CT on each patient (I know you are thinking about the decision to scan in each, as your natural medicine brains will not allow you to avoid pursuing a diagnoses). But, hopefully this post will instead stimulate you to think about another very important question. Namely, how do you summarize the literature for an anxious, perhaps tearful family, and how do you communicate your recommendations to them, given the evidence that suggests when to scan, in the face of mounting concerns about the exposure to ionizing radiation.
Check out the next post where I'll share my thoughts. until then I'm interested in seeing what all of you are thinking.
So, if you haven't already done so , go ahead and read the seminal Lancet 2009 article.
Kuppermann - Lancet, 2009
OK, welcome back... I ended up seeing three patients, all of whom presented by smacking their heads on hard surfaces. I've changed their names and ages to protect the innocent, and to avoid the wrath of Hungry Hungry HIPAA.
- The first patient was a school aged male whose bike failed him, and whose helmet was hanging in his garage. He ended up introducing his occiput to the pavement, though his recollection of this event was foggy at best. His sensorium was mired in the same fog.
- The second was an infant, who despite her mother's best efforts, wriggled free from her arms and fell to the concrete below. The baby cried immediately, and aside from the large hematoma on her forehead, looked great.
- Sensing a theme, you might wager that the third cranium contacted concrete in a concussive cacophony (sorry about the alliteration). It did, but 2 days ago. A visit to an urgent care, and a 'medical' neighbor later - had filled the family with enough information to seek care at my ED as they wondered whether or not their robust toddler needed a head CT.
There is a delicate balance between managing the anxieties and expectations of a parent, when they are (justly so) legitimately worried about their child's well-being. Perhaps they are a medical professional themselves, and armed with just enough (mis)information to make them worry more than they should. Or maybe, they consulted Dr. Google, or worse, Dr. facebook in that back alley clinic that would make Dr. Nick Riviera of the Simpson's blush.
Go ahead and think for a moment about whether or not you would order a head CT on each patient (I know you are thinking about the decision to scan in each, as your natural medicine brains will not allow you to avoid pursuing a diagnoses). But, hopefully this post will instead stimulate you to think about another very important question. Namely, how do you summarize the literature for an anxious, perhaps tearful family, and how do you communicate your recommendations to them, given the evidence that suggests when to scan, in the face of mounting concerns about the exposure to ionizing radiation.
Check out the next post where I'll share my thoughts. until then I'm interested in seeing what all of you are thinking.
Tuesday, May 29, 2012
Video laryngoscopy with the GlideScope
Check out this video detailing the use of the GlideScope for endotracheal intubation
Video laryngoscopy with the Stroz C-MAC
Here is a video detailing use of the Storz C-MAC system for video laryngoscopy
Final Leaderboard Update
Thanks to all who participated! As announced at today's Noon Conference, the winner of the 2012 #PEMTwitterTriviaContest was...
@Bedingaj

Coming in at 2nd place we found
@paulbunchmd
Followed by the 3rd place finisher
@MarlinaLovett
@Bedingaj

Coming in at 2nd place we found
@paulbunchmd
Followed by the 3rd place finisher
@MarlinaLovett
Introduction to Video Laryngoscopy
Check out this video as a follow up to last week's lecture on RSI and video laryngoscopy by Gary Geis.
Saturday, May 26, 2012
Spinal cord injury syndromes
Central cord syndrome
Incomplete spinal cord injury
Weakness in the arms with relative sparing of the legs with variable sensory loss
Ischemia, hemorrhage, or necrosis involving the central portions of the spinal cord
May be seen in recovery from spinal shock due to prolonged swelling around or near the vertebrae, causing pressure on the cord. Can be transient or permanent.
Anterior cord syndrome
Associated with flexion type injuries to the cervical spine
Damage to the anterior portion of the spinal cord and/or anterior spinal artery
Below the level of injury motor function, pain sensation, and temperature sensation are lost
Touch, position and vibration are intact
Posterior cord syndrome
Posterior portion of the spinal cord and/or posterior spinal artery
Loss of proprioception and epicritic sensation (e.g. stereognosis, graphesthesia) below the level of injury
Motor, pain, and sensitivity to light touch are intact
Brown-Séquard syndrome
Hemisectioned or lateral injury side (penetrating trauma)
Ipsilateral side loss of motor function, proprioception, vibration, and light touch
Contralateral side loss of pain, temperature, and crude touch sensations
NEXUS and Canadian C-spine rule: When to get films
Think about what you do in the ED? Do you recognize how following studies have impacted your practice?
National Emergency X-Radiography Utilization Study
Multicenter, prospective, observational study of patients with blunt trauma for whom cervical spine X-rays were obtained.
Get C-spine films if:
http://www.nejm.org/doi/full/10.1056/NEJM200007133430203
Canadian C-spine rule
A prospective cohort study in Canada evaluating patients with head or neck trrauma.
Radiography in high risk factors
Assess range of motion in low-risk factors. If none of the following are present and the patient can actively rotate 45 degrees to left and right, then C-spine films may not be needed.
National Emergency X-Radiography Utilization Study
Multicenter, prospective, observational study of patients with blunt trauma for whom cervical spine X-rays were obtained.
Get C-spine films if:
- Patients with abnormal neurologic examination
- Distracting or painful injury (like a femur fracture)
- Depressed or altered mental status
- Intoxication
- Midline cervical tenderness should get an X-Ray
http://www.nejm.org/doi/full/10.1056/NEJM200007133430203
Canadian C-spine rule
A prospective cohort study in Canada evaluating patients with head or neck trrauma.
Radiography in high risk factors
- Dangerous mechanism
- Paresthesias
Assess range of motion in low-risk factors. If none of the following are present and the patient can actively rotate 45 degrees to left and right, then C-spine films may not be needed.
- Simple rear-end MVC
- Sitting position in the ED
- Ambulatory at any time since injury
- Delayed onset neck pain
- Absence of midline C-spine tenderness
Friday, May 25, 2012
Pop! goes the appendix
Perforation is more likely in younger kids because:
1. More thin walled appendix, predisposing to early perforation
2. Younger children can’t communicate as well, resulting in prolonged symptoms before diagnosis
3. The level of suspicion for appendicitis is lower in younger age groups
Pro-Tip: In addition, appendicitis can progress to peritonitis quicker in infants, because they have a less well developed omentum, and thus cannot contain infection as well.
1. More thin walled appendix, predisposing to early perforation
2. Younger children can’t communicate as well, resulting in prolonged symptoms before diagnosis
3. The level of suspicion for appendicitis is lower in younger age groups
Pro-Tip: In addition, appendicitis can progress to peritonitis quicker in infants, because they have a less well developed omentum, and thus cannot contain infection as well.
Pediatric Appendicitis Score
Pediatric
Appendicitis Score
(1
point) anorexia
(1
point) fever
(1
point) nausea/vomiting
(1
point) migration of pain
(2
points) pain with cough, percussion, or hopping
(2
points) RLQ tenderness
(1
point) Leukocytosis (WBC > 10,000)
(1
point) Left shift (ANC >6750)
- 10 point scale incorporating history, physical and lab components
- Initial study (Samuels, 2002) with N = 1170
- Prospective cohort age 4-15 with abdominal pain suggestive of appendicitis
- Cutoff of >=6 provides 1.00 sensitivity and 0.92 specificity
- Logistic regression to determine best fit of diagnostic variables for sum of true-positive and true-negative results (total joint probability for a single cutoff)
- Validation studies have shown better performance at the ends of the spectrum (using 2 cutoffs)
- Validated prospectively and retrospectivelyIn ages > 1
- Using various combinations of cutpoints
- High risk scores (> 7) had a specificity of 95-98%
- Low risk scores (<3) had a negative predictive value of 98%
- Moderate risk scores indicated the need for further imaging
- Use of the PAS would have decreased the need for imaging
Leaderboard Update - Day 18
We are closing in on the conclusion of the #PEMTwitterTriviaContest. The leader board as of this morning...
1st @Bedingaj
2nd @paulbunchmd
3rd @MarlinaLovett
Wednesday, May 23, 2012
Do it FAST!
FAST is a Focused Assessment with Sonography for Trauma that utilizes bedside ultrasound to rapidly identify intraperitoneal pericardial hemorrhage in trauma patients.
It is indicated in abdominal trauma patients who are hypotensive and/or who are unable to provide a reliable history. It is an adjunct to the primary survey (ABCs). In adults a positive FAST (blood in the abdomen/pericardium) means a trip to the OR for laparotomy. In children small amount of intraperitoneal blood is not as significant as in adults, and many can be managed conservatively.
Here are the locations for FAST
Perihepatic


Perisplenic

Pelvis

Pericardium


Images courtesy of Trauma.org - This is a great overview of FAST - Check it out here
It is indicated in abdominal trauma patients who are hypotensive and/or who are unable to provide a reliable history. It is an adjunct to the primary survey (ABCs). In adults a positive FAST (blood in the abdomen/pericardium) means a trip to the OR for laparotomy. In children small amount of intraperitoneal blood is not as significant as in adults, and many can be managed conservatively.
Here are the locations for FAST
Perihepatic


Perisplenic

Pelvis

Pericardium


Images courtesy of Trauma.org - This is a great overview of FAST - Check it out here
Clavicle fractures - to fix or not to fix
In children 10 years of age and under 90% of clavicle fractures occur in the middle third, 60 percent
of which are nondisplaced. Above age 10, the majority are displaced
(as in adults). immobilization with sling and swathe for 3-4 weeks is generally sufficient for most uncomplicated fractures.
Outpatient Orthopedic referral is recommended for:
Outpatient Orthopedic referral is recommended for:
- Patients with a completely displaced clavicle fracture, which is defined as displacement greater than one bone width.
- Shortening greater than 18 mm in males and 14 mm in females because of the risk of significant morbidity, including local tenderness, numbness, pain when lying on the affected side, impaired range of motion, impaired strength, and cosmetic abnormalities
- Comminuted fracture
Emergent referral is required for:
- open fractures
- neurovascular compromise
- tenting of the skin (skin stretched tautly over a displaced fracture)
An open fracture should be suspected anytime
there is a break in the skin near a fracture site. After puncturing the skin
during the initial injury, fractured bone ends often retract under the skin and
cannot be seen with simple inspection. If respiratory compromise or hemodynamic
instability exists, serious injury to intrathoracic or other structures should
be suspected and immediately addressed. proximal third clavicle fractures are generally associated with more significant trauma, and have a higher potential for internal injuries.
Traditionally the management his followed the dictum "If both ends of the bone are in the same room, then sling and swathe alone is sufficient." New evidence has suggested otherwise.There may be advantages to repairing select medial fractures in the OR. See this article for more information.
http://www.ncbi.nlm.nih.gov/pubmed/18803979
http://www.ncbi.nlm.nih.gov/pubmed/18803979
Tuesday, May 22, 2012
Kocher Criteria: Helping to differentiate septic hip versus transient synovitis
Kocher criteria for a child with a painful hip, suspected to have septic arthritis:
1) non-weight-bearing on affected side
2) sedimentation rate greater than 40 mm/hr
3) fever
4) WBC >12,000
Criteria met and probability child has septic arthritis
4/4 -- 99%
3/4 -- 93%
2/4 -- 40%
1/4 -- 3%
http://jbjs.org/article.aspx?Volume=86&page=1629
1) non-weight-bearing on affected side
2) sedimentation rate greater than 40 mm/hr
3) fever
4) WBC >12,000
Criteria met and probability child has septic arthritis
4/4 -- 99%
3/4 -- 93%
2/4 -- 40%
1/4 -- 3%
http://jbjs.org/article.aspx?Volume=86&page=1629
Monday, May 21, 2012
Ow my elbow! A bit about supracondylar fractures of the humerus
 Type I
Type INondisplaced or minally displaced fracture
On the lateral view: anterior humeral line remains intact but a posterior fat pad sign may be present
Treatment
Treated w/ immobilization in long arm posterior splint w/ elbow flexed and outpatient Ortho follow up

Type II
Posterior cortex remains intact, making it a greenstick fracture technically
Treatment:
Require adequate reduction and percutaneous pinning in many instances
Consult Ortho immediately

Type III
Displaced with no cortical contact
Treatment
Immediate Ortho consult - This will need to go to the OR in most instances
Day 15 Leaderboard
There's a change at the top of the #PEMTwitterTriviaContest Leaderboard, as @Bedingaj has surged ahead with an impressive weekend stint. There's still plenty of time to catch up though, with competitors hot on her tail.
1st: @Bedingaj
2nd: @paulbunchmd
3rd: @MarlinaLovett
In the hunt:
@GreggKottyan
@ziggy7652
@preetir85
@TarekAlsaied
@amyocon24
@dbailey4
@7hillsandariver
@AnotherLynLee
Friday, May 18, 2012
One pill can kill!
These medicines could potentially be fatal in a single dose to a 10kg toddler
- Benzocaine
- Camphor
- Chloroquine
- Clonidine
- Cyclic antidepressants
- Diphenoxylate/atropine (Lomotil)
- LIndane
- Methadone (and other opioids)
- Methyl salicylate (oil of wintergreen)
- Oral hypoglycemics
- Quinidine
- Propranolol
- Theophylline
- Thioridizine
- Verapamil
Thursday, May 17, 2012
Suturing and tetanus prophylaxis
Suturing Guidelines
For
Uncontaminated, Uncomplicated Lacerations
LET
(Lidocaine-Epinephrine-Tetracaine)
-
Works in ~ 30 minutes
-
Use only on broken skin (won’t work on intact skin)
-
Don’t use on mucous membranes (risk of toxicity)
- CAUTION
with fingertips, toes, penis, nose, or pinna b/c of epi
EMLA
(Eutectic Mixture of Local Anesthetic)
ELA-max
Use only on intact skin (NOT on lacerations!)
ELA-max
Use only on intact skin (NOT on lacerations!)
ELA-max
works in 30 minutes, EMLA takes an hour
OK
to use on areas of distal circulation because no epi
Lidocaine
1%
lidocaine = 10 mg/ml
2% lidocaine = 20 mg/ml
2% lidocaine = 20 mg/ml
Max
dose - lidocaine WITH epi = 7 mg/kg (up to 280 mg)
Max
dose - lidocaine WITHOUT epi = 4 mg/kg (up to 280 mg)
w/ epi DO NOT
use on fingertips, toes, penis, nose, pinna
To buffer
with bicarb: 1:10 solution with 8.4% sodium bicarbonate
(9ml of lidocaine + 1ml bicarb)
(9ml of lidocaine + 1ml bicarb)
Location
|
Percutaneous (Skin)
|
Deep (Dermal)
|
Days to removal
(percutaneous only)
|
Scalp
|
Staples
or
5-0/4-0
Prolene/Ethilon
|
4-0
Vicryl/Chromic Gut
|
7-10
|
Ear
|
6-0
Prolene/Ethilon – SEE NOTE*
|
5-7
|
|
Eyelid
|
7-0/6-0
Prolene/Ethilon. If low on lid,
consult Ophtho.
|
5-7
|
|
Eyebrow
|
6-0/5-0
Prolene/Ethilon
|
5-0
Vicryl/Chromic Gut
|
5-7
|
Nose
|
6-0
Prolene/Ethilon - SEE NOTE*
|
5-0
Vicryl/Chromic Gut
|
5-7
|
Lip
|
6-0
Prolene/Ethilon
|
5-0
Vicryl/Chromic Gut
|
5-7
|
Oral
mucosa
|
---
|
4-0 or 5-0 Vicryl/Chromic Gut
|
---
|
Tongue
|
Suture
if significant step-off or through and through laceration
|
||
Other
face/
forehead
|
6-0
Prolene/Ethilon – SEE NOTE*
|
5-0
Vicryl/Chromic Gut
|
4-5
|
Trunk
|
5-0/4-0
Prolene/Ethilon
|
3-0
Vicryl/Chromic Gut
|
8-10
(Chest/Abd)
12-14
(Back)
|
Extremities
|
6-0/5-0/4-0
Prolene/Ethilon
|
4-0
Vicryl/ Chromic Gut
|
8-10
|
Hand
|
6-0/5-0
Chromic
|
5-0
Vicryl/ Chromic Gut
|
8-10;
10-12 (tip)
|
Extensor tendon
|
Refer
to plastic surgeon
|
||
Foot/sole
|
4-0/3-0
Prolene/Ethilon
|
4-0
Vicryl/ Chromic Gut
|
12-14
|
Vagina
|
---
|
4-0
Vicryl/Chromic Gut
|
---
|
Scrotum
|
---
|
5-0
Vicryl/Chromic Gut
|
---
|
Penis
|
5-0
Prolene/Chromic
|
---
|
7
|
*Consider
use of Fast Absorbing Gut (5-0/6-0) on Ear, Eyelid, Eyebrow, Nose, Lip and Face
if anticipated difficulty with suture removal (Note: follow up still required
for wound evaluation)
NOTE: If cartilage involved, strongly consider
plastic surgery consult. Always treat with
antibiotics
NOTE: If human/animal bite, cleanse, dress, treat
with antibiotics, and follow-up with Plastics.
If tendons are involved, start antibiotics and consult Plastics. See ‘Bugs and Drugs’ section (page 63-64) for
specific treatment guidelines.
Tetanus administration
Immunization history
|
Dirty,
Tetanus prone: >6 hrs since injury;
stellate or avulsion injury; missile, crush, burn, frostbite; >1 cm deep;
devitalized /contaminated.
|
Clean,
Non-tetanus prone: ≤6 hours since injury; linear injury; sharp surface (glass,
knife); ≤1 cm deep; No devitalized or contaminants
|
||
TdaP (Adacel)
|
TIG
|
TdaP (Adacel)
|
TIG
|
|
Unknown or <3 doses
|
Yes
|
Yes
|
Yes
|
No
|
3 or more doses
|
No,
unless >5 yrs since booster
|
No
|
No,
unless >10 yrs since booster
|
No
|
Subscribe to:
Posts (Atom)